Instructions
Attached:
-SOAP Example to use as a guide
– SOAP Template to fill out for this assignment.
Instructions:
-Choose one skin condition graphic to document your assignment in the SOAP note (Subjective, Objective, Assessment, and Plan).
– Use the attached Comprehensive SOAP Template for guidance. Remember that NOT ALL comprehensive SOAP data is needed in every patient case. ONLY fill out what is important for your diagnosis.
-Use clinical terminologies to explain the physical characteristics featured in the graphic.
-Formulate a differential diagnosis of three to five possible conditions for the skin graphic that you chose.
-Determine which is most likely to be the correct diagnosis and explain your reasoning using at least three different references.
Solution
Comprehensive SOAP: Integumentary
Patient Initials: AB Age: 27 years Gender: Female
SUBJECTIVE DATA:
Chief Complaint (CC): “I have dark stretch marks on my abdomen.”
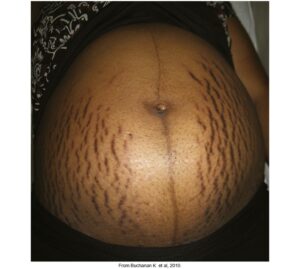
History of Present Illness (HPI): Alice Brenda is a 27-year-old Hispanic female who has visited the clinic for her usual antenatal care. AB is in her 36th week of pregnancy. She denies having any health issues today. However, she is concerned about the increasing number of dark stretch marks on her abdomen as shown in picture number 2. The marks started to appear during her fifth week of pregnancy but they were not as many as they are today.
Besides, they have become darker than they were four months ago. AB reports that this is her first pregnancy and that she has never seen such marks on any parts of her body before. She denies using systemic steroids or potent corticosteroids. The marks do not occur with any other symptoms/discomfort such as itching or redness. She is not using any medications at the moment to manage the stretch marks. AB is on folic acid and iron supplements which she has been taking since she began her antenatal care.
Medications:
- Iron supplements
- Folic acid supplements
Allergies:
Amoxicillin – rash
Denies food allergies
Past Medical History (PMH):
1.) Pneumonia
2.) Tonsilitis
3.) Cellulitis
Past Surgical History (PSH):
Denies
Sexual/Reproductive History:
AB identifies as a female. Menarche was at age 13. She used to have a regular menstrual cycle taking 28-30 days. Her menses normally last 4 days when she is not pregnant and they occur with minimal cramping. AB denies using any method of contraption before her pregnancy. She had a pap smear test before she became pregnant and results were negative.
Personal/Social History:
AB has been married to her husband for 2 years. They live together in the city. AB works as a nurse at community hospital. She does not smoke cigarettes and denies consuming alcohol. She drinks 2 cups of coffee every morning. She denies illicit drug use.
Immunization History:
Influenza Vaccination 09/2/2021
Tdap 2/8/2019
PNV 18/9/2020
Covid Vaccine #1 7/8/2021 #2 8/10/2021 AstraZeneca
Significant Family History:
AB’s father is 54 years old. He was recently diagnosed with type 2 diabetes mellitus which is well controlled. Her mother is 49 years old and she is healthy. She has 2 sisters (17 and 14 years) who are both healthy. Her paternal and maternal grandparents are all deceased.
Lifestyle:
AB eats vegetables and fruits together with her daily meals. Her typical diet is mainly Hispanic diet. She drinks four glasses of water per day and reports walking to work every day. She denies going to the gym.
Review of Systems:
General: No chills or night sweats; reports recent weight gains as the fetus continues to grow; reports occasional fatigue; Denies nausea, vomiting, or fever
HEENT: Denies physical head injury. Denies a headache. Does not report redness and pain in the issues. No vision issues reported. Does not report a history of cataracts. Denies using contact glasses. Does not report double vision or excessive tearing. Denies ear pain, hearing loss, ear infection, or hearing in the ears. No nasal stuffiness reported. Does not report nasal discharge or obstruction. No recent changes in smell reported. Denies a history of nasal infections. No mouth ulcers, pain, or dryness reported. Denies hoarseness of the throat. Denies a history of mouth or throat infections.
Neck: Denies swelling, pain, injury, compression, or history of disc disease.
Breasts: Denies redness, rashes, masses, or a history of lesions. Reports soreness or mild pain in the breasts since the first trimester of pregnancy.
Respiratory: Denies difficulty breathing. Reports occasional coughs. No hemoptysis reported. Denies pleuritic chest pain, wheezing, or cyanosis. Reports a history of pneumonia. Denies a history of tuberculosis.
CV: Denies heart murmur, chest discomfort, or palpitations; no history of arrhythmias, orthopnea, paroxysmal nocturnal dyspnea, edema, or claudication. Her last ECG was 3 months ago.
GI: Denies abdominal pain, constipation, and diarrhea. No history of dysphagia or heartburn. Denies vomiting or nausea, excessive belching or a history of gallbladder problems.
GU: Reports changes in her urinary pattern with increased frequency observed in the recent weeks. AB identifies as a female. She denies a history of sexually transmitted diseases. She has been sexually active for 2 years now.
MS: Denies joint stiffness or pains. No joint swelling, joint tenderness, backache, limitations of motion, or a history of fractures reported. Denies a history of arthritis or join-related complications.
Psych: Reports psychological distress due to the increasing number of stretch marks on her abdomen. Denies history of anxiety or depression. Does not report sleep disturbance, delusions or mental health history. Denies suicidal/homicidal attempt or ideation.
Neuro: Denies seizures, tingling, tremors, or numbness of limbs. Denies headaches muscle atrophy, dizziness, or memory changes.
Integument/Heme/Lymph: Reports an increasing number of dark stretch marks on her abdomen. Denies skin rashes, lesions, dryness, or scaling. Denies a history of nail thickening or thinning of the hair.
Endocrine: She does not report polyuria/polyphagia/polydipsia. Denies alopecia, heat or cold intolerances, or abnormal sweating at night.
Allergic/Immunologic: AB develops rashes on her body when she uses amoxicillin. She denies food allergies.
OBJECTIVE DATA
Physical Exam:
Blood pressure; 130/80, temperature; 36.8 degree Celsius, pulse; 92 beats per minute, respiratory rate; 20 breaths per minute, weight; 158.4 pounds.
General: AB is attentive and keeps eye contact during conversation.
HEENT: No evidence of trauma. It is normocephalic. Absence of depressions or palpable masses. Hair is of normal texture. No signs of alopecia. No evidence of lesions or swelling of the eyelids. No signs of hemorrhage of conjunctivae. No evidence of icterus on sclerae. No evidence of discharge or blockage in the ear canal. No tenderness or edema on the external ear and ear canal. A pale grey color is observed in the tympanic membrane. No signs of nasal hemorrhage. Nasal mucosa is hairy, pink, and moist. The nasal septum is at the midline positioned. No evidence of sores, lesions, or ulcers in the oral mucosa. Oral mucosa is moist and pink with good dentition on the gums. The pharynx is pink in color without with signs of edema or tonsillar exudates.
Neck: No evidence of swelling. No goitre.
Chest/Lungs: No evidence of deformities on inspection. Normal breath sounds, wheezes, crackles, rubs, or rhonchi on auscultation. No fremitus detected on palpation.
Heart/Peripheral Vascular: Normal heart rate, S1, S2, without galloping, murmurs, or rubbing. No noise on a bilateral basis. Midclavicular PMI visible, 5th intercostal region, no heaves, lifts, or excitement. No evidence of edema on the periphery. Varied bilateral peripheral pulses, capillary refill less than 3 seconds.
ABD: Distended as evidence of pregnancy. Evidence of dark striae on the distended abdomen. The striae are widespread on both sides of the abdomen.
Musculoskeletal: Normal gait, good balance, no evidence of muscle rigidity. Muscle strength on all joints is 5/5. Lower and upper limbs are sensitive to touch and pricking. Reflexes are 2+.
Neuro: AB is attentive and able to concentrate. Has a good level of consciousness. No evidence of language, speech, or memory issues. Full EOM’s on cranial nerves II-IX. The nerves are intact. Visual fields observed.
Skin: The skin is warm and smooth. Evidence of dark striae on the distended abdomen. The striae are widespread on both sides of the abdomen.
Diagnostics/Lab Tests and Results:
Davey’s scoring- A score of 6 indicates severe stretching of the abdominal skin
Dermoscopy-Evidence of increased melanization/hyperpigmentation in the striae
Assessment:
Differential Diagnosis (DDx):
- Striae gravidarum
- Steroid atrophy
- Abdominal scars
Primary Diagnoses:
1.) Striae gravidarum
References
Ball, J. W., Dains, J. E., Flynn, J. A., Solomon, B. S., & Stewart, R. W. (2019). Seidel’s guide to physical examination (9th ed.). St. Louis, MO: Elsevier Mosby.
Bickley, L. (2018). Bates guide to physical examination and history taking (12th ed.). Philadelphia, PA: Wolters Kluwer.
Farahnik, B., Park, K., Kroumpouzos, G., & Murase, J. (2016). Striae gravidarum: Risk factors, prevention, and management. International Journal of Women’s Dermatology, 3(2), 77–85. https://doi.org/10.1016/j.ijwd.2016.11.001